 OSHA issued its final rule on beryllium, which is a metal that can cause cancer and other health issues when inhaled or absorbed into the skin, on Jan. 9, 2017.
OSHA issued its final rule on beryllium, which is a metal that can cause cancer and other health issues when inhaled or absorbed into the skin, on Jan. 9, 2017.
Because the rule was initially met with opposition and controversy, the agency delayed its enforcement on several occasions. In June 2017, OSHA also announced that it would not enforce the final rule’s standards, other than the new Permissible Exposure Level (PEL)and Short Term Exposure Limit (STEL), for construction or shipyard employers. OSHA also issued a direct final rule to clarify portions of the final rule on May 7, 2018.
On July 14, 2020, the final rule for the general industry beryllium was revised and went into effect Sept. 14, 2020. The construction and shipyard standards were also revised on Aug. 31, 2020 and went into effect on Sept. 30, 2020. Both standards were amended to clarify certain provisions and simplify or improve compliance.
Links and Resources
- OSHA Interim Enforcement Guidance 2020 Final Beryllium Standard\
- OSHA Occupational Chemical Database
- National Institute of Occupational Safety and Health (NIOSH)
- Workplace Safety and Health Topic- Beryllium
- Preventing Sensitization and Disease from Beryllium Exposure
- International Chemical Safety Cards (ICSC)
- Beryllium and beryllium compounds FAQs website
|
Highlights
- OSHA’s final rule reduced the PEL for beryllium to 0.2 micrograms per cubic meter of air (μg/m3).
- The final rule also set a 2.0 μg/m3 STEL and a 0.1 μg/m3 action level.
- The new PEL and STEL apply in the general, construction and shipyard industries.
- General industry employers must also implement certain workersafety measures.
|
Important Dates
July 14, 2020
Final ruled revised for the general industry beryllium standard.
Aug. 31, 2020
Final rule revised for the construction and shipyard beryllium standards.
Health Effects of Beryllium
Exposure to beryllium via inhalation of airborne beryllium or skin contact with beryllium-containing dust, fume, mist or solutions can cause health effects. Under OSHA’s beryllium standards (29 CFR 1910.1024; 29 CFR 1915.1024; 29 CFR 1926.1124), employers must reduce exposures to airborne beryllium to or below the beryllium PELs through engineering controls to the extent feasible, supplemented by respirators where all feasible controls are not sufficient to reduce exposures to or below the PELs. In addition, personal protective clothing and equipment (PPE) (e.g., gloves and shoe covers) is required when airborne exposures can exceed the PEL or STEL or there is the potential for skin exposure.
OSHA also requires employers provide workers with detailed training on the health effects of beryllium. Training must include, among other things: information on the health hazards associated with airborne exposure to and dermal contact with beryllium, including the signs and symptoms of CBD; information on the purpose, proper selection, fitting, proper use, and limitations of personal protective clothing and equipment, including respirators; any protective measures workers can take to protect themselves from airborne or skin exposure to beryllium (including personal hygiene practices); and the purpose and description of the medical surveillance program and medical removal protection.
The following information describes the primary health effects associated with exposure to beryllium, medical testing and surveillance requirements, and possible treatment for beryllium-related health effects.
Primary Health Effects Associated with Exposure to Beryllium
The most common health effects associated with overexposure to beryllium in the workplace include beryllium sensitization, chronic beryllium disease (CBD) and lung cancer.
Beryllium sensitization: Beryllium sensitization is the activation of the body’s immune response to beryllium. Beryllium sensitization can result from inhalation or skin exposure to beryllium dust, fume, mist or solutions. While no clinical symptoms may be associated with sensitization, a sensitized worker is at risk of developing CBD when inhalation exposure to beryllium has occurred.
Chronic beryllium disease: CBD is a chronic granulomatous lung disease caused by inhaling airborne beryllium after becoming sensitized to beryllium. Some common symptoms of CBD are shortness of breath, unexplained coughing, fatigue, weight loss, fever and night sweats. CBD can result from inhalation exposure to beryllium at levels below the current OSHA PEL (0.2 μg/m3). Progression of CBD can vary among individuals. For instance, after initial exposure to beryllium, some workers may quickly develop signs and severe symptoms of CBD. Others may not experience signs and symptoms until months or years after initial exposure. The symptoms can sometimes worsen even after the worker has been removed from exposure. CBD can progress to a chronic obstructive lung disorder, resulting in loss of quality of life and the potential for decreased life expectancy (for additional information see section on Treatment below).
CBD shares many signs and symptoms with pulmonary sarcoidosis, a granulomatous lung disease of unknown cause or origin. Without appropriate diagnosis, CBD may be difficult to distinguish from sarcoidosis.
Lung cancer: Based on numerous studies in occupational settings, OSHA has determined that occupational exposure to beryllium causes lung cancer in humans. In addition, the International Agency for Research on Cancer (IARC) classifies beryllium as a Group 1 carcinogen (carcinogenic to humans) and the National Toxicology Program (NTP) lists beryllium as a known human carcinogen.
Acute beryllium disease (ABD): ABD is a rapid onset form of chemical pneumonia that results from breathing high airborne concentrations of beryllium. ABD is generally associated with exposure to beryllium levels at or above 100 μg/m3 and may be fatal in 10% of cases. ABD is extremely rare in the workplace today due to more stringent exposure controls implemented following occupational and environmental standards set in the 1970s.
Medical Surveillance
The purpose of medical surveillance is to detect and eliminate the underlying causes of observed health effects from hazards. Medical surveillance programs can contribute to the success of workplace health and safety programs by identifying potential problem areas and verifying the effectiveness of existing control and prevention programs.
Under the beryllium standards (29 CFR 1910.1024; 29 CFR 1915.1024; 29 CFR 1926.1024), OSHA requires employers to offer medical surveillance to workers within 30 days of determining that the worker meets one of the following conditions: is or is reasonably expected to be exposed above the action level of 0.1 μg/m3 for 30 days in a year; show signs or symptoms of CBD; were exposed to beryllium during an emergency; or have received a recommendation for continued medical surveillance from a physician or other licensed health care professional (PLHCP) from the most recent exam (see Beryllium Standard: Guidance on Medical Surveillance for Beryllium Exposed Workers). Employees may opt out of the medical surveillance program if they so choose. The medical surveillance requirements within the beryllium standards include the following provisions:
Employers must offer medical surveillance to a worker within 30 days of meeting the criteria set forth in paragraph (k)(2)(i), and at least every two years thereafter for those who continue to meet the criteria in paragraph (k)(1). The standards also specify medical examination at the termination of employment (see paragraph (k)(2)(iii) in the standards). The medical examination must include:
- Medical and work history with emphasis on past and present airborne exposure to or dermal contact with beryllium, smoking history and any history of respiratory system dysfunction
- Physical examination with emphasis on the respiratory system
- Physical examination for skin rashes
- Pulmonary function tests
- BeLPT2 (or other equivalent test)
- Any other test deemed appropriate by the PLHCP (including low-dose CT scan3)
|
OSHA requires that employers provide certain information to the PLHCP. This information includes:
- A copy of the standard
- A description of the employee’s former and current duties that relate to the employee’s airborne exposure to and dermal contact with beryllium
- The employee’s former and current levels of airborne exposure
- A description of any PPE, used by the employee, including respirators, that includes when and how long these were used
- Information from records of employment-related medical examinations previously provided to the employee, currently within the control of the employer, after obtaining written consent from the employee
|
OSHA requires the employer to ensure that the employee receives a written medical opinion from the licensed physician within 30 days of the medical examination. The written opinion must include:
- The results of the medical examination (including whether the employee has any detected medical condition that may place the employee at increased risk from further airborne exposure or any medical conditions related to airborne exposure that require further evaluation or treatment)
- Any recommendations on the employee’s use of PPE or respirators
- Any limitations on the employee’s airborne beryllium exposure
- Any recommendation for referral to a CBD diagnostic center, continued medical surveillance or medical removal
|
OSHA also requires the employer receive a medical opinion form the licensed physician. The written medical opinion must include:
- The date of the examination
- Statements that the results of the examination were explained to the worker (4) and that the examination met the requirements of the beryllium standard
- Any recommended limitations on the worker’s use of respirators, protective clothing or equipment
- If the employee provides written authorization, the written opinion must also contain any recommended limitations on the worker’s airborne exposure to beryllium
|
If the worker is either confirmed positive for beryllium sensitization or CBD or a licensed physician has determined it appropriate, and the worker provides written authorization, OSHA requires employers to provide:
- A referral to a CBD diagnostic center (5)
- Continued medical surveillance
- Medical removal (upon request by worker)
|
The BeLPT – Beryllium sensitization may be detected with the beryllium lymphocyte proliferation test (BeLPT), a blood test for measuring the immune response to beryllium. The observation of beryllium-specific lymphocyte proliferation in an individual peripheral blood sample indicates an abnormal response and may indicate beryllium sensitization. There is some concern about the accuracy of the BeLPT. A single BeLPT has been reported to have a false-positive rate of about 1% (Middleton et al., 2008). Many programs therefore rely on a second test to confirm a positive result (NAS, 2008), which has been reported to reduce the false positive test result rate to about 0.02% (Middleton et al., 2008).
Another way to measure the accuracy of a test such as the BeLPT is to measure its positive predictive value (PPV). The PPV is the probability that a person with a positive result has the disease or condition being measured. To address some criticism regarding the PPV of the BeLPT, Middleton et al. (2011) conducted another study to evaluate borderline results from BeLPT testing. Table 1 below shows the PPV for the BeLPT using either two abnormal results, one borderline and one abnormal result, or three borderline results (Middleton et al., 2008 and 2011):
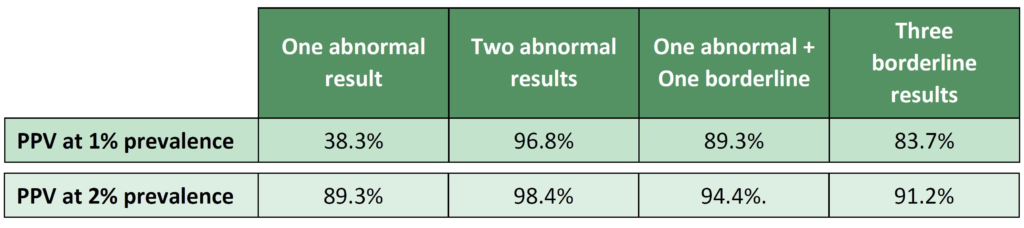
Based on this information OSHA considers a worker positive for sensitization with either two abnormal results, on abnormal and one borderline, or three borderline results. CBD is generally confirmed when it can be shown there is a history of beryllium exposure; positive histopathology findings in the lung (e.g., fiber-optic bronchoscopy, X-ray, CT scan or lung biopsy); and beryllium sensitization.
Workers found to be sensitized to beryllium are at risk for developing CBD and in need of continuing medical follow-up. OSHA requires employers to offer sensitized workers a physical examination every two years performed under the direction of a licensed physician.
For more information see OSHA’s Safety and Health Topics page on medical screening and surveillance.
Treatment
There is no cure for CBD. Treatment for CBD can vary for each patient, depending on the severity of the disease. Treatment may include corticosteroids, oxygen and other means to ease symptoms or slow the disease progression.
Source: Occupational Safety and Health Administration
This Compliance Overview is not intended to be exhaustive nor should any discussion or opinions be construed as legal advice. Readers should contact legal counsel for legal advice. Design © 2021 Zywave, Inc. All rights reserved.

